“ME/CFS is a biological illness, not a psychologic disorder. Patients with ME/CFS are neither malingering nor seeking secondary gain”
US Centers for Disease Control and Prevention
Key stats
30m
individual cases globally (pre pandemic)
Long Covid prevalence rates that meet ME diagnostic criteria are not yet quantified
250k
healthcare worker cases globally (pre pandemic)
Long Covid prevalence rates that meet ME diagnostic criteria are not yet quantified
9000+
article assessment corroborating regulatory failure of medical norms
US Institute of Medicine assessment of ME systemic exertion intolerance
100%
regulatory failure of medical norms
BPS papers ranked 87% very low quality, 13% low quality in UK NICE assessment
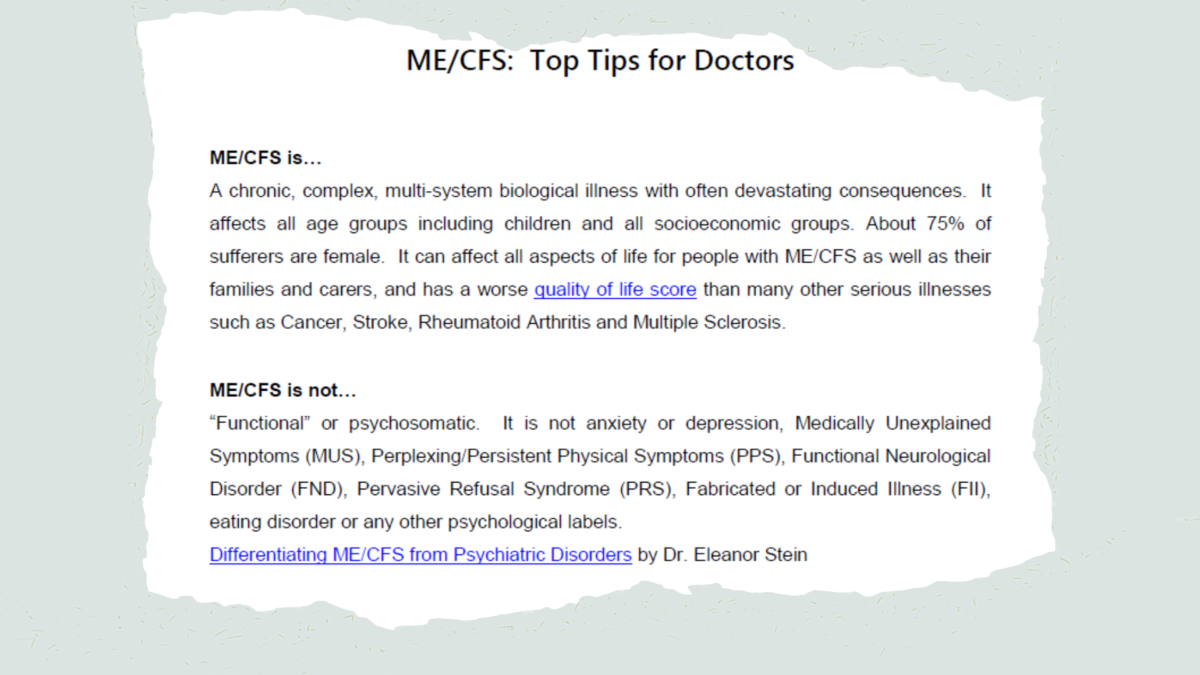
Myalgic encephalomyelitis is a common, complex, chronic, multi-system physical disease that already affected over 30 million people globally pre-pandemic. Classified by the World Health Organization ICD and SNOMED-CT as a neurological condition, the disease causes unusually severe disability and most often manifests post-virally (onset can be masked by life circumstances). It can also affect people of any age or demographic, including children.
ME is sometimes referred to by the problematic legacy term “chronic fatigue syndrome” or the acronym ME/CFS. The incomplete and stigmatising nature of the term chronic fatigue syndrome is frequently compared to previously misapplied “hysterical paralysis” terminology used for multiple sclerosis patients. The double-barrelled acronym ME/CFS exists to bridge past terminological failures and the original disease name, meaning many professionals and patients are more comfortable with the term ME.
ME/CFS ≠ “fatigue” alone (idiopathic, unexplained)
ME/CFS ≠ “chronic fatigue” alone (idiopathic, unexplained, FND, MUS, PPS)
ME/CFS ≠ post-viral fatigue syndrome alone
ME/CFS has distinct diagnostic criteria, multi-system symptomatology, scientific consensus and legal status
Normalised mismanagement can accelerate progression through these diagnoses, with a diagnostic audit trail documenting liability-generating harm
Serious disease
ME patients are not just unusually neglected. Quality of life scores are shocking – worse than nearly all conditions encountered in primary and secondary care (with little difference in emotional or mental health, despite repeated confirmation of ME as a greater physical disability). They are unusually vulnerable, often with little physical capacity to address issues that affect them, implying the need for additional care in clinical frontline services and administrative contexts.
Quantified quality of life comparators vs ME in the above statement include HIV/AIDS, heart disease, congestive heart failure, cancer, stroke, end stage renal failure, lung disease, type 2 diabetes, osteoarthritis, multiple sclerosis, epilepsy, eosinophilic gastroenteritis, cystic fibrosis, sciatica and other maladies.
Diagnostic criteria
ME benefits from straightforward diagnostic criteria that are clear. Common patterns are often evident e.g. post-viral onset. Future research may potentially split these into cohorts.
The belief that ME has no diagnostic marker and is a diagnosis of exclusion (similar to Parkinsons) is a misrepresentation. Exclusion is critical to avoid misdiagnosis of mental health or other physical diseases as ME, but systemic exertion intolerance characterised by Post Exertional Malaise (PEM) / Post Exertional Symptom Exacerbation (PESE) / Post Exertional Neuroimmune Exhaustion (PENE) is a cardinal symptom. Abnormalities are observable in controlled research contexts with the two day cardio-pulmonary exercise tests (an inappropriate risk if only for diagnosis) and in metabolic and other findings.
The most appropriate diagnostic criteria are the Institute of Medicine Criteria, the International Consensus Criteria and the Canadian Consensus Criteria. The field has previously been undermined by lax criteria that scaled misdiagnoses and contributed to ongoing stigma and discrimination. The Oxford, Fukuda and NICE 2007 criteria should not be used, and research studies using those criteria do not apply to ME.
Treatment and management
High quality evidence-based care is worse than rare – the disease is largely unaddressed or mismanaged, at best. Despite being common and having clear diagnostic criteria, the empirical consensus documents unusually low levels of understanding amongst medical professionals of ME epidemiology, disability and management. Current norms versus ME are analogous to prejudices that were previously psychologised versus other physical conditions, such as multiple sclerosis, asthma or autism.
There is no cure or clear path to recovery. Evidence-implied management and risk-minimisation strategies exist, corroborated by general empirical findings that are compatible with patient experience. Individual symptoms can sometimes be treatable, although the systemic exertion intolerance that distinguishes ME from other illnesses must be managed to avoid post-exertional malaise. Psychological support is repeatedly found to be curatively irrelevant. Such support can help patients cope with the debilitating chronic illness experience, as with any chronic illness, but should in no way be promoted as curative for ME.
Scientific clarity
There is broad scientific consensus regarding:
- what is known about ME/CFS
- what ME/CFS is not
- what is not known
- evidenced and broad areas for future research
The US CDC has thus removed dangerously irrelevant biopsychosocial guidance – they are now explicit that the disease is biophysical, serious, multisystemic and not due to malingering. This is further reflected in the US Institute of Medicine review of over 9000 scientific papers and articles.
The research base that underlies medical norms has faced a 100% regulatory failure rate, with a UK National Institute of Health and Care Excellence assessment of biopsychosocial papers ranking 87% very low quality and 13% low quality. This is a corollary of their incompatibility with the scientific consensus.
Nonetheless, not enough is known about predisposition, precipitating onset factors nor progression. The market for ideation and human capital has suffered from stunted research-economics, whether in commercial or grant-allocation terms. This is attributable to socio-medical norms that undermine this market, directly and indirectly.
Public health outcomes and clinical liability
The poor public health outcomes from normalised misconceptions are grave – even prior to the shortcomings revealed by the pandemic. Even where there is goodwill, medical norms still regularly run entirely contrary to scientific consensus and are enabled by failed regulatory assessments. This in turn undermines other practitioners’ knowledge and public policy formulation – extending costly misconceptions into client industries, such as pharmaceuticals and insurance.
These weaknesses and failings risk patient harm and regulatory compliance repercussions. At best, they undermine trust across patient and client relationships. At worse, they generate substantial medico-legal risk. They also contribute directly to inaccurate media narratives that perpetuate socio-medical harm, beyond medical care and into families and workplaces.