Section 1.16 of the NICE ME/CFS Guideline requires that health and social care providers ensure that all staff delivering care to people with ME/CFS have an understanding of the patient experience.
Doctors with M.E. asked the CFS/ME Research Collaborative Patient Advisory Group (CMRC PAG) what patients make of the new NICE guideline. They shared the statement below.
PAG Summary Statement
The CMRC PAG welcomes the new NICE guideline for ME/CFS as a significant step forward for people with ME/CFS. The guideline is patient centred, and we feel our voices have been heard.
There is clear acknowledgement in the guideline that ME/CFS is a multi-system disorder with myriad symptoms that vary in occurrence and severity throughout the patient population. Importantly, the guideline recognises Post Exertional Malaise as a defining symptom of the condition, along with disturbed sleep and cognitive difficulties. The descriptors of ME/CFS severity make clear that even for those who are mildly affected this is a life-changing diagnosis. For those who are very severely affected the impact is catastrophic.
We particularly welcome the removal of any recommendation for fixed, incremental exercise or activity programs such as graded exercise therapy (GET). It is right that the guideline committee acknowledged the substantial qualitative evidence of patient harm due to this intervention.There is widespread lack of awareness of the evidence showing an abnormal cellular response to exertion in ME/CFS patients, characterised by post-exertional symptom exacerbation and reduced physical capacity over the following days, weeks, or months. This has been demonstrated in repeat 24-hour exercise physiology testing; patients with ME/CFS have reduced cardiopulmonary function, lower anaerobic threshold, and increased acidosis when they repeat exercise the next day, in comparison with controls.
We welcome the recommendation for a personalised care and support plan, which takes into account factors such as the provision of mobility aids and adaptations to help patients access medical care. In the past, many patients have been denied mobility aids and discharged when too unwell to attend appointments.
We also welcome the provision of mobility aids when needed; this will help patients maximise their independence and better manage their limited energy. Patients should not have to battle for such basic support.
However, we feel the guideline is ambiguous with regards to justification for inclusion of CBT. While it is right that CBT has been demoted from ‘treatment’ to a supportive role, we are unclear why CBT has preferential status over other supportive interventions, especially as the guideline rightly refutes the foundational principles of so-called ME-CBT.
Although the guideline is a vast improvement on its predecessor, it is disheartening to see that patients, who often have a significantly more impacted quality of life in comparison to patients with other diseases and cancer, are essentially left with self-management strategies. It is imperative that biomedical research into this illness is drastically increased so that patients can one day be offered safe and effective treatments within the clinic. Until that time, we hope this guideline enables patients to be met with empathy and understanding, rather than disbelief and disdain.
Individual Patient Reactions
Gemma
As a child I was diagnosed with ME/CFS. I was always seen as an odd case. I could manage school, but nothing else really. However I was told to maintain a routine, not to nap during the day and to try and keep going. To see such a marked change in the new guidelines gives me huge hope for any children and teenagers that are now having to deal with this path. I have managed, by finding my own way and sacrificing a lot that teenagers, young adults etc take for granted, and having an amazing support network. This condition is definitely not all in my head, and it’s amazing to finally see the people in power acknowledging that!
Gemma, PhD Student
Howard
My name is Howard. I was 33 and a mature postgraduate law student when ME/CFS came calling in 1997. I was a fit, motivated,self starting, active high achiever with a part-time military career and good prospects. After ME/CFS hit, I spent 7 months bedbound in an unending state of permanent fatigue, not able to eat more than one complete meal and only able to walk a few metres. In the 23 years since I have barely ever worked, as any form of trivial activity wiped and continues to wipe me out for hours or days. I have only made a partial recovery, and without a cure I am stuck in limbo, permanently reliant on state aid for my daily life. I never asked for this, I never wanted this – but it happened anyway.
I lost everything: friends; motivation; my sanity; my future; my independence; my hope. I learned the hard way how to cope and adjust to my new life. How to pace myself, how to prioritise tasks and which bad advice to ignore – of which there was a lot from people who thought, in their ignorance, their bad advice was helpful. Until I went to a properly set up ME/CFS clinic over ten years after I first became ill, which survived on a shoestring NHS budget that kept being cut, I was not properly diagnosed in detail and what I had always suspected was the case, but my GP would not say, was confirmed. Even then, all I was offered was Cognitive Behavioural Therapy (how to think yourself better) and Graded Exercise Therapy (I was still quite active, but pacing myself, I felt it would be a waste), and Vitamin B and Folic Acid supplements. That was it. That’s all there was. And that’s pretty much all there still is without properly funded biomedical research to find effective treatments.
Dom
Three-and-a-half years ago I was subjected to a bizarre and degrading consultation with a so-called ME/CFS expert, who I later found out had been involved with the now debunked PACE trial. He was not at all interested in my symptoms, which at that time were increasing in severity, and instead proceeded to take my life history, before recommending I consider ‘doing things badly on purpose’ and ‘doing fun and frivolous things’, and a sham therapy known as the Lightning Process.
The new NICE guideline explicitly recommends against the Lightning Process. It also confirms what I knew at that time; that I had a serious multisystem illness which I wouldn’t be able to exercise or think my way out of. The guideline is a huge step forward, but it’s also a stark reminder of the lack of appropriate treatment. Only a substantial commitment to biomedical research into this illness will change that. In the meantime, the guideline should help patients be taken seriously and be appropriately supported as they navigate this horrendous illness.
Dom, 34, ex-research scientist
Simon
5 Years ago I was diagnosed with ME/CFS after a viral infection. I was lucky, I had a very supportive GP who believed me. Even so, I feel my life has been stolen. I spend my days estimating how much energy I have left, and how much I can devote to a particular task. Every morning I wake feeling exhausted. The exercise I used to enjoy is no longer accessible. Every task must be broken down into manageable chunks with rest breaks. I’m lucky, I have a very good GP and I’m only mildly affected.
Simon, 57, ex-IT consultant
More NICE ME/CFS Guideline 2021 Content
Doctors with M.E. proposes a simple solution to ensure success of the UK’s ME/CFS Delivery Plan. Following the then Secretary of State for Health and Social Care Sajid Javid’s announcement of a cross-nation delivery plan for ME/CFS, work has been underway at the Department of Health and Social Care to identify issues and find solutions.…
Replacing Working Group Glass Ceilings with Enforceable Minimal Standards (clickable video chapters below and on YouTube site) Further to our recent statement regarding major UK announcements, the above presentation provides the solution to concerns about new DHSC ME/CFS Delivery Planning mechanisms and final implementation. Current glass ceilings will limit success of this new process and…
Doctors with M.E Director and colleagues respond regarding the ignored importance of unpaid carers Doctors with M.E. Director, Dr. Nina Muirhead, has co-authored a BMJ Rapid Response regarding the topic of unpaid carers of people with ME. This important factor is largely ignored by the 2021 NICE ME/CFS Guidelines, the recent APPG report and the…
Doctors with M.E. warmly welcomes the UK Secretary of State for Health and Social Care’s recent inauguration of cross-nation delivery planning processes with his Chief Scientific Officer, Professor Lucy Chappell. Sajid Javid’s intervention on social media in the case of Maeve O’Neill was strikingly poignant, touching the hearts of many patients, carers and medics. We…
Psychiatry and Psychology Working GroupDr Crowder BSc (hons) MB ChB FRANZCP, Associate, DwMEYochai Re’em, M.D., Associate, DwME | Website | Twitter What is ME/CFS? ME/CFS is a chronic, complex, multi-system biological illness with often devastating consequences. It affects all age groups including children, and all social classes. About 75% of sufferers are female. It has…
When faced with a life changing, devastating chronic illness with no cure in a young person, doctors often don’t know what to do. Doctors with M.E. has produced guidance for GPs, but what do patients want? We asked patients to share examples of when doctors got it right. It is heartening to read this collection…
Contents Overview Myalgic Encephalomyelitis (ME), also known as Chronic Fatigue Syndrome (CFS), is a chronic, complex, multi-system biological illness with often devastating consequences. It affects all age groups including children and all social classes. About 75% of sufferers are female. It has a worse quality of life score than many other serious illnesses including cancer,…
Doctors with M.E. stands ready to work with partners and organisations to bring medical education up-to-date and assist in developing the right services for ME/CFS patients. “The new guideline represents a positive and total paradigm change, uniting around the science, official disease classification and medico-legal compliance implications.” “This translation of scientific knowledge into clinical practice…
Doctors with M.E. recognise the contributions to clinical practice, research literature and scientific innovation of our latest Honorary Fellows, Caroline Kingdon and Dr. William Weir. Their contributions have accelerated the quality of empirical work and grounded the literature in frontline clinical relevance. This experience has most recently culminated in their roles as full Committee Members…
A call for the Royal College of Paediatrics and Child Health to explain undermining of scientific review Doctors with M.E. Associate, Neurodisability Paediatrician and representative on the JLA Priority Setting Partnership Steering Group, Dr. Ben Marsh, has publicly written to the President of The Royal College of Paediatrics and Child Health (RCPCH). He requested an explanation for the College’s…
The current NICE debacle and extraordinary deviation from normal procedure and published protocol is further evidence of institutionalised discrimination by large sections of the UK medical establishment. That one professional and patient group should be treated in a manner at odds with clear and growing scientific knowledge would be unacceptable in any other disease. Yet…
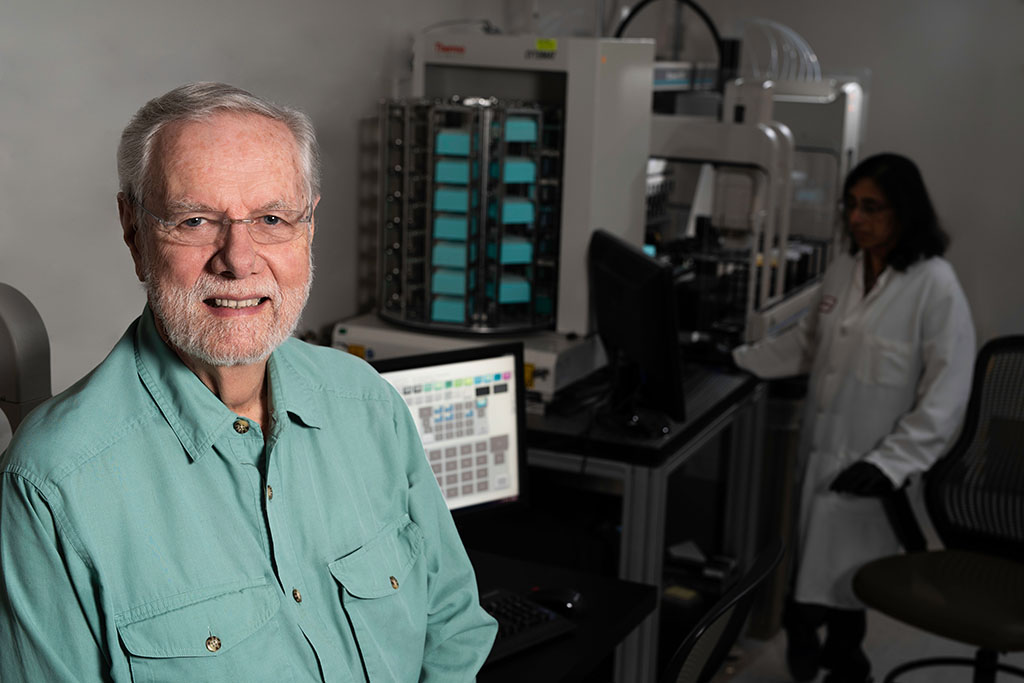
Doctors with M.E. Honorary Fellow Professor Ron Davis has issued a powerful statement condemning the failure of the UK National Institute of Clinical and Care Excellence to maintain its independence. He describes how it has instead accommodated vested interests, which perpetuate low standards and contra-scientific medical belief systems. “It is a travesty that NICE is…
Doctors with M.E. Board, Fellows & Associates are co-signatories to a public letter written by Dr. David Tuller of the Center of Global Public Health at the University of California, Berkeley. The letter writes to urge NICE to publish the new ME/CFS guideline. It is signed by scientists, clinicians, academics and other experts from the…
ME, Long Covid and the NICE Guideline 2021 Delay Doctors with M.E. Director, Dr. Nina Muirhead, and Doctors with M.E Honorary Fellow and Action for ME Medical Advisor, Dr. David Strain, discuss ME/CFS, Long Covid, the NICE guideline delay and the need for more education and resources in an interview on BBC Radio 4 Woman’s…
A call for change in the face of long-standing regulatory failure The following public communication from our Governance Board regards the opportunity for a new “Medical Regulatory Agency”, ready for the post-brexit and the machine learning digital eras. The letter also contains background pertaining to long-standing regulatory failure, unlawful medical norms, contra-scientific medical belief systems and…
We are very disappointed to hear of the ‘pause’ in publication of the NICE ME/CFS Guideline, already delayed in April. Following the hard work of the Guideline Development Group, we received news of the further delay of guideline publication with both dismay and profound concern for practitioners, their organisations and patients. Continued delay or deviation…
The following expert testimony was provided to the NICE ME/CFS Guidelines Committee by Professor Jonathan Edwards. It regards the difficulties of conducting trials in ME/CFS and the implications of not accounting for these. The difficulties of conducting intervention trials for the treatment of myalgic encephalomyelitis / chronic fatigue syndrome Summary testimony Therapeutic trials for ME/CFS…
The following expert testimony was provided to the NICE ME/CFS Guidelines Committee by Doctors with M.E. Director, Dr. Nina Muirhead. It regards the problematic context of lacking information, education and support for health and social care professionals. Information, education and support for health and social care professionals providing care for people with ME/CFS. Summary testimony…
Is it just me, or is the BMJ’s take on those NICE guideline committee resignations maybe a little biased? The BMJ are reporting that four members of NICE’s guideline committee on ME/CFS have stood down. One is the medical advisor of the ME Association, who stated yesterday that he found it too difficult to combine…
Further to our position statement on the 2021 NICE guideline update, Doctors with M.E. has joined the call for NICE to ensure that unconsulted changes are not injected, as these would avoid scrutiny by the scientific community. DwME considers the 2021 NICE guideline to be a watershed moment in the history of ME/CFS medical care…
On the 10th of November 2020, the National Institute for Health and Care Excellence (NICE) published its draft updated guideline on the diagnosis and management of myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome (ME/CFS). NICE has updated its 2007 recommendations on the use of psycho-behavioural treatments for ME/CFS, concluding that Graded Exercise Therapy (GET) should no…