Contents
Overview
Myalgic Encephalomyelitis (ME), also known as Chronic Fatigue Syndrome (CFS), is a chronic, complex, multi-system biological illness with often devastating consequences. It affects all age groups including children and all social classes. About 75% of sufferers are female. It has a worse quality of life score than many other serious illnesses including cancer, stroke, rheumatoid arthritis and MS, and it can affect all aspects of life for both people with ME/CFS and their families and carers.
The hallmark symptom of ME/CFS is Post Exertional Malaise (PEM). This is the exacerbation of illness that results when a patient’s energy limit is exceeded. It involves a worsening of all symptoms, can include the emergence of new symptoms or symptoms not normally present, is prolonged, and out of proportion to the trigger. Onset can be delayed by up to several days and the exacerbation in illness can last days, weeks, months or years.
Patients with ME/CFS have impaired energy metabolism at the cellular level and struggle to produce ATP molecules to power activity. They also have measurable abnormalities in immune, neurological, cardiovascular, endocrine, gastrointestinal and other functions. People with ME/CFS must reduce and adapt their activities to conserve energy. This includes all types of activity including physical, cognitive, social and emotional activity, and takes into account overall level of activity. Management consists of teaching patients to stay within their energy limits to avoid triggering Post Exertional Malaise. Pacing activity and rest throughout the day can help manage symptoms and prevent deterioration.
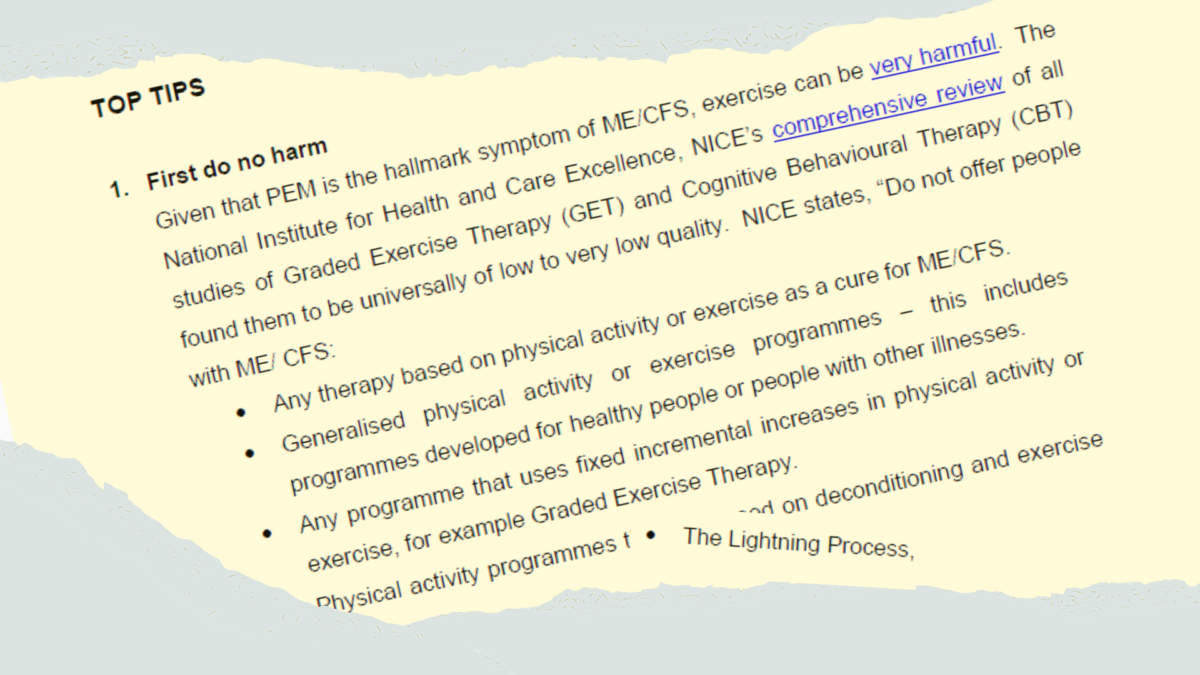
ME/CFS is not psychosomatic, and psychological therapies will not cure the disease. NICE clearly states, “Do not offer people with ME/CFS:
- Any therapy based on physical activity or exercise as a cure for ME/CFS.
- Generalised physical activity or exercise programmes – this includes programmes developed for healthy people or people with other illnesses.
- Any programme that uses fixed incremental increases in physical activity or exercise, for example Graded Exercise Therapy.
- Physical activity programmes that are based on deconditioning and exercise avoidance theories as perpetuating ME/CFS.
- The Lightning Process, or therapies based on it.”
pg. 31, section 1.11.14 / pg. 39, section 1.12.27
Graded exercise has caused much harm to people with ME/CFS. Talking therapies such as CBT can at best provide psychological support, and at worst contribute to harm by consuming precious energy or misinforming patients. NICE states that CBT does not cure ME/CFS and must not assume people have abnormal illness beliefs and behaviours as an underlying cause of their ME/CFS.
Diagnosing ME/CFS
Suspect ME/CFS in adults who have been symptomatic for six weeks, and children who have been symptomatic for four weeks. The four main symptoms should be present, and the person’s ability to engage in occupational, educational, social or personal activities should be significantly reduced from pre-illness levels. Advise patients to manage their activities to stay within their energy limit. They should rest and convalesce as needed and not push through their symptoms. Meanwhile, perform a thorough workup to rule out other potential causes and explanations for symptoms. At three months, if symptoms persist and are not due to another cause, diagnose ME/CFS.
ME/CFS is a positive diagnosis based on its clinical features. While it is important to rule out other potential causes for symptoms and to look for comorbidities, it is not a diagnosis of exclusion. NICE states that the four main symptoms of ME/CFS are:
- Debilitating fatigue that is worsened by activity, is not caused by excessive cognitive, physical, emotional or social exertion, and is not significantly relieved by rest.
- Post Exertional Malaise.
- Unrefreshing sleep or sleep disturbance.
- Cognitive difficulties or ‘brain fog’.
Associated symptoms are:
- Orthostatic intolerance, autonomic dysfunction, dizziness, palpitations, fainting, nausea on standing or sitting upright from a reclining position.
- Temperature hypersensitivity resulting in profuse sweating, chills, hot flushes, or feeling very cold.
- Neuromuscular symptoms, including twitching and myoclonic jerks.
- Flu-like symptoms, including sore throat, tender glands, nausea, chills or muscle aches.
- Intolerance to alcohol, or to certain foods and chemicals.
- Heightened sensory sensitivities, including to light, sound, touch, taste and smell.
- Pain, including pain on touch, myalgia, headaches, eye pain, abdominal pain or joint pain without acute redness, swelling or effusion.
ME/CFS patients can sometimes report “air hunger” or appear to hyperventilate. This is easily confused with anxiety, but is likely to be due to lactic acidosis following over-exertion. A damaged aerobic respiratory system forces ME/CFS patients to rely on their anaerobic system to generate energy, which builds up high levels of lactic acid. This also explains the prolonged myalgia that they experience after minor exertion.
Principles of care
While there is as yet no cure for ME/CFS, compassionate care can make a huge difference to the patient experience. ME/CFS patients have traditionally been treated with disbelief, disdain, neglect and even abuse, including in “specialist” NHS clinics. Many patients have found healthcare encounters so traumatic that they avoid it altogether, to the detriment of their health. NICE now recommends a patient centred approach. A doctor who is willing to work with the patient to manage his/her symptoms is invaluable. Doctors should:
1. Believe your patients
2. Learn about ME/CFS
Register at Doctors with M.E. and make use of the educational opportunities on offer. Medical knowledge is extremely poor, with misconceptions about ME/CFS widespread among practicing clinicians. By learning about ME/CFS, you will understand that the huge list of disparate and seemingly extreme symptoms that patients report are real and not imagined, and how you may help with them. You will know the common comorbidities that can be present, which could be treated in their own right.
3. Teach pacing
Teach patients to pace their activities and advise them of the importance of rest. An occupational therapist who understands ME/CFS can be invaluable in teaching pacing techniques and providing aids and adaptations that help conserve energy.
4. Provide symptomatic treatment
Target the most troublesome symptoms first, and slowly, we may be able to make life a little easier for our patients. When prescribing medications, start low and go slow. ME/CFS patients are highly susceptible to side effects so a cautious approach is advised but we should not let this stop us from doing what we can to ease symptoms.
5. Be accessible
For many patients, the exertion of attending a medical appointment will trigger Post Exertional Malaise, and for others who are bedbound it isn’t an option at all. In order for these patients to receive any medical care providers should offer alternative arrangements such as telephone or video consultations and home visits. Provide a named contact so that patients know how to get help when needed.
Care should be taken to respect patients’ hypersensitivities and allergies. This may mean keeping voices low, using minimum lighting, minimising touch, and not wearing perfumes or other products that the patients may be allergic to. These limitations present a further barrier to care as most health care environments are unsuitable for severely affected ME patients and will worsen their illness.
6. Support applications for financial support and social care
ME/CFS has been shown to be more debilitating than many other serious illnesses including cancer, stroke, rheumatoid arthritis and MS. This is with little difference in emotional or mental health, despite repeated confirmation of ME as a greater physical disability in QALY terms. Only a minority are able to work and most of these work part-time and have to sacrifice social and other activities to sustain the energy requirements of their work. Therefore, access to any help to which patients are entitled is very important. The severely and very severely affected patients may need much practical help and social care.
7. Support accommodations at work and in education
ME/CFS is a recognised disability with rights to reasonable adjustments. Accommodations can include modifications to the work environment, rest facilities, shorter working hours, working from home and transport or parking arrangements. In many circumstances patients may be entitled to assistance via the Access to Work scheme to enable them to continue doing their jobs.
For children and young people, consider education at home where required, making use of online resources, communication tools, home schooling and flexible or hybrid arrangements, to provide equal access to education as much as is possible. ME/CFS is the single greatest cause of long-term sickness absence in UK schools, therefore it is important to find solutions which minimise the impact of this disease on educational attainment and long-term outcomes.
8. Arrange nutritional support where required
Severely ill ME/CFS patients can struggle to maintain their nutrition for a variety of reasons, including muscle weakness or paralysis, difficulty swallowing, nausea or abdominal pain, food intolerances or allergies and Mast Cell Activation Syndrome. Screen for undiagnosed gastrointestinal disorders, such as Coeliac disease. Some patients need tube feeding. Be alert to this possibility and refer early for nutritional assessment and support to prevent deterioration from avoidable malnutrition.
9. Review regularly
Review ME/CFS patients at least annually and review children at least every six months. People with ME/CFS can develop other medical problems like anyone else, and this gets more likely as they get older. Evaluate and investigate new symptoms or change in symptomology to determine if they are due to ME/CFS or another condition. Ensure patients have access to routine screening and checks, and that they receive appropriate vaccinations.
10. Refer for specialist care
Refer patients to an ME/CFS specialist team which includes medically trained physicians, GPs or Paediatricians, as well as allied health care professionals specialising in ME/CFS.
11. Protect patients from Safeguarding misadventures
Countless families in the UK of children with ME/CFS have faced suspicion or been wrongfully investigated for abuse or neglect, at the hands of poorly informed practitioners. The number of such cases is in triple figures and still rising. Both adults and children have been known to be forcibly admitted into mental institutions for their ME/CFS. Patients are frequently misdiagnosed or given various psychiatric/psychological labels. There is oft diagnosed in the UK a questionable condition called Pervasive Refusal Syndrome. This “diagnosis” is found neither in the ICD-10, ICD-11 nor DSM-5. Its “symptoms” resemble severe ME, and its “treatment” is psychiatric admission, psychological therapy and rehabilitation.
Other inappropriate labels for ME/CFS include Functional Neurological Disorder (FND), Fabricated or Induced Illness (FII), Medically Unexplained Symptoms (MUS), Perplexing/Persistent Physical Symptoms and eating disorder. NICE advises that if abuse or neglect is suspected, we should involve professionals who have proper knowledge and experience of ME/CFS as soon as possible. NICE also stresses that the following observations in patients with suspected or confirmed ME/CFS are not necessarily indications of abuse or neglect:
- Physical symptoms that do not fit a commonly recognised illness pattern.
- More than one child or family member having ME/CFS.
- Disagreeing with, declining or withdrawing from any part of their care and support plan, either by them or by their parents or carers on their behalf.
- Parents or carers acting as advocates and communicating on their behalf.
- Reduced or non-attendance at school.
The UK context
Old medical beliefs and harmful treatments
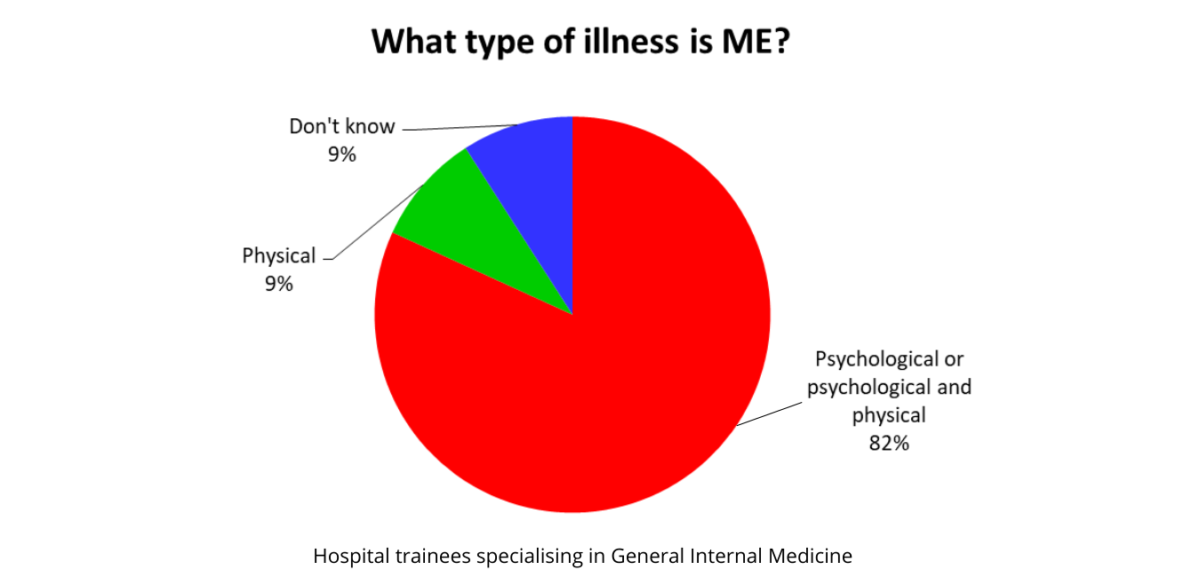
At the present time, the psychological narrative of ME/CFS is predominant in the UK. The majority of practicing clinicians have little knowledge or understanding of the illness, as illustrated by this audit of a group of General Internal Medicine trainees. Many NHS specialist clinics have not yet caught up with the new NICE guideline and the latest scientific knowledge. They continue to operate on the basis of outdated psychological theories, offering treatments known to be harmful or otherwise persisting with a misguided focus on “rehabilitation”, i.e. increasing exercise or activity, instead of staying within energy limits.
Some clinics appear unaware of the low recovery rate in ME/CFS of no more than 5%, and continue to promote the goal of recovery. Anecdotal evidence suggests that when patients elect not to return to a clinic, or become too ill to attend having been harmed by their treatments, they are discharged and recorded as successful outcomes. In the UK, iatrogenic harm from non-pharmacological therapies is not routinely recorded. Data can also be further confounded by high misdiagnosis rates.
Treatment programmes offered in UK clinics may have different names such as Graded Activity Management or be described as “individualised”, but any programme which does not incorporate proper understanding of the principles of energy management in ME/CFS will be unhelpful and most likely harmful. An urgent roll out of education is needed across all medical specialties to bring the NHS up-to-date.
What this means for General Practitioners
GPs may need to take greater ownership of their ME/CFS patients, and be prepared to look after those who are unable to access a specialist clinic, do not wish to be referred to a specialist clinic, or do not feel that their experience at a specialist clinic has been helpful. NICE states that patients have the right to decline any treatment or therapy without it affecting any other aspect of their care.
GPs who find themselves in this position should not fear. Remember that things are not any worse today than yesterday, and patients do not expect us to become experts overnight. All they want is a doctor who is willing to help, and if that means taking the time to learn about a particular aspect of their illness, they will gladly wait. Remember that many ME/CFS patients have been sick for a very long time. A short wait in order to get meaningful help is of minor concern to them. Because of the sad history of neglect and dismissal that these patients have suffered, people with ME/CFS are most appreciative of just basic compassion.
Many patients will be able to provide us with relevant information and resources. The lack of help from the NHS has meant patients have had to help themselves. Keep an open mind and we may find learning about ME/CFS is not as difficult as we imagined. There is plenty that we do know about ME/CFS, and plenty of educational resources available. Doctors with M.E. can help bring everyone up to speed.
A career opportunity
ME/CFS is an emerging and exciting field looking for pioneers. The new NICE guideline and the avalanche of new cases as a result of the Covid-19 pandemic hopefully heralds greater recognition and funding. The need for accessible community based services for ME/CFS is urgent and growing, regardless of specialist secondary care services dealing with other complications of Covid-19 infection.
Why not set up an ME/CFS service yourselves? Or link up with existing clinics to provide a more community based model of care. All one needs to embark on this journey is an enquiring mind and a listening ear. ME/CFS offers a unique career opportunity for the driven. With its unusually appreciative patients, intriguing clinical features and fascinating ongoing research, it promises to be a particularly rewarding career. Doctors with M.E. stands ready to assist providers in the development of responsive and accessible services for this neglected patient group, as described by NICE.